Understanding the Biological Mechanisms of SoftWave
Click Here or call 800-382-5879 for a Customized SoftWave Estimate.
For clinic owners and therapists, the management of chronic pain often presents a significant barrier to positive outcomes.
Traditional modalities typically address the mechanical or muscular aspects of injury, yet in many patients, pain persists due to underlying neuro-immune factors.
SoftWave Tissue Regeneration Technologies (TRT) has gained traction in the clinical space not merely as a symptom-management tool, but as a biological intervention.
To understand its value in a practice, one must understand the cellular mechanisms through which it operates.
This article reviews the biological pathways SoftWave utilizes to modulate pain, inflammation, and tissue regeneration.
1. The Clinical Context: Pain as a Neuro-Immune Problem
To treat chronic pain effectively, it must be recognized as a complex feedback loop involving three distinct systems:
-
Peripheral Nerves: Specifically, the hyper-excitability of A-delta and C fibers.
-
Central Sensitization: Maladaptive changes in the spinal cord and brain (“pain memory”).
-
The Immune System: The presence of macrophages, microglia, and cytokines.
Chronic pain cycles are sustained by pro-inflammatory mediators such as TNF-α, IL-1β, and IL-6, along with neuropeptides like Substance P and CGRP. Effective treatment must interrupt this chemical and electrical loop.
Healthcare Providers - Request SoftWave Demonstration
"*" indicates required fields
2. Mechanism of Action: Multimodal Pain Modulation
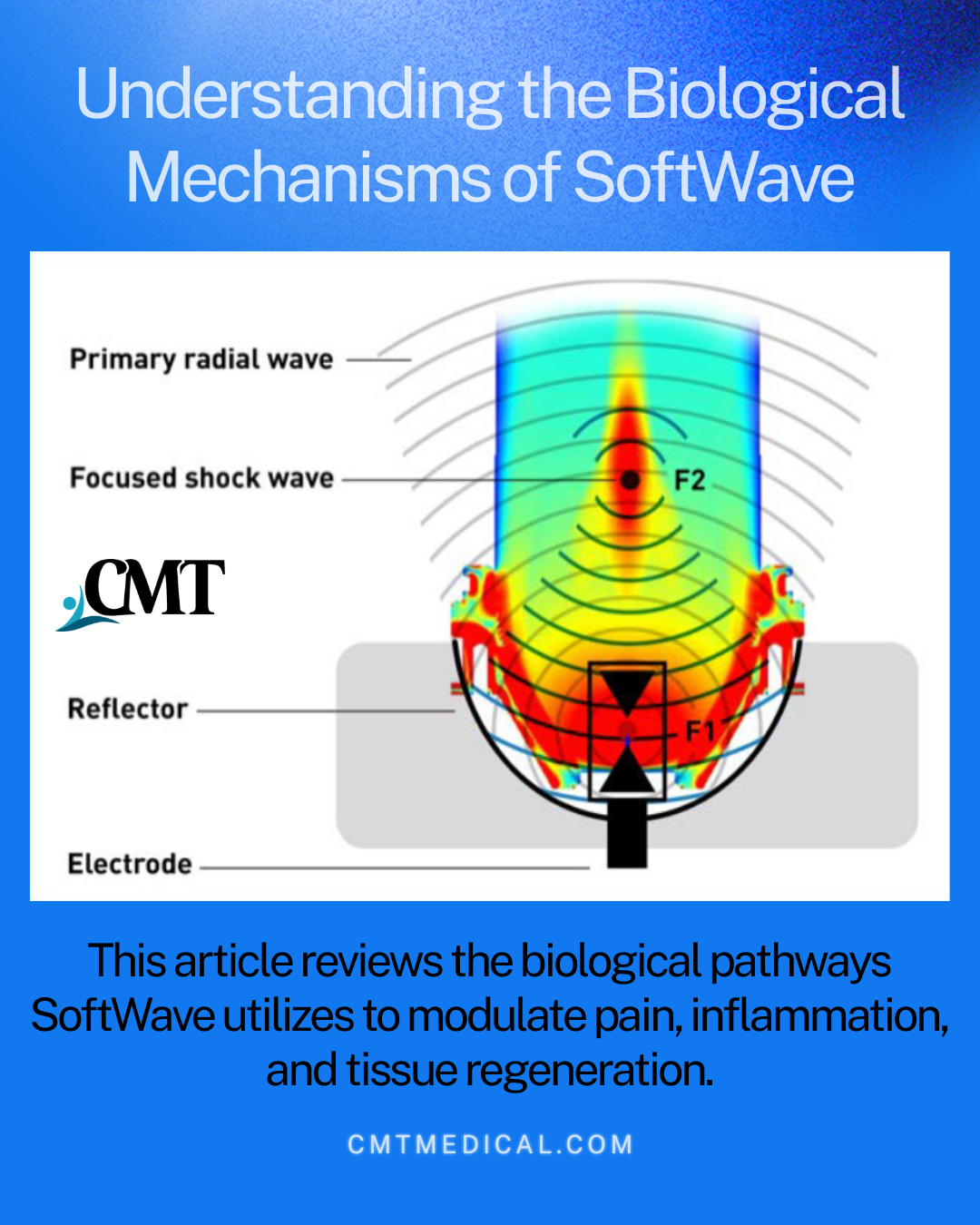
SoftWave therapy utilizes unfocused electrohydraulic shockwaves to trigger responses across three biological levels simultaneously.
Direct Neural Effects
The immediate analgesia often observed during treatment is attributed to the “Hyper-Stimulation Analgesia” theory. The acoustic waves impact the peripheral nervous system by:
-
Disrupting Pain Signaling: Temporarily disrupting synaptic transmission.
-
Reducing Excitability: Decreasing the firing rate of unmyelinated C-fibers, which are responsible for slow, chronic pain.
-
Altering Neurotransmission: Reducing the local concentration of Substance P and CGRP, the neuropeptides responsible for transmitting pain signals and driving neurogenic inflammation.
Neuro-Immune Modulation (The M1/M2 Shift)
A critical differentiator of SoftWave is its ability to modulate the immune response rather than simply suppressing it.
-
Macrophage Polarization: Mechanical stimuli can induce a phenotypic shift in macrophages from M1 (pro-inflammatory/destructive) to M2 (anti-inflammatory/regenerative).
-
Cytokine Regulation: This shift results in a downregulation of pro-inflammatory cytokines and an upregulation of anti-inflammatory mediators like IL-10, effectively dampening the chemical engine of chronic pain.
Central Mechanisms
By altering peripheral signaling and reducing the constant nociceptive input to the dorsal horn, the therapy can help disrupt maladaptive “pain memory” circuits. This allows clinicians to address central sensitization, treating the chronic pain state even after the original tissue injury has theoretically healed.
 3. Regenerative Effects: Why Results Last
3. Regenerative Effects: Why Results Last
While symptom relief improves patient compliance, tissue repair drives long-term outcomes. SoftWave initiates mechanotransduction—the conversion of mechanical stress into biochemical responses.
This process stimulates the release of growth factors (VEGF, IGF, BMP-2), leading to:
-
Angiogenesis: The formation of new blood vessels, improving microcirculation and oxygenation in hypoxic tissue.
-
Tissue Remodeling: Enhanced collagen synthesis and organization.
-
Stem Cell Activation: Activation of progenitor and stem-cell-related pathways to repair damaged structures.
The pain relief is durable because it is tied to an improvement in the physiological health of the tissue.
4. Clinical Application and Safety profile
SoftWave has demonstrated clinical utility across a range of musculoskeletal and neuropathic conditions, including:
-
Plantar fasciitis and tendinopathies
-
Chronic low back pain and myofascial syndromes
-
Chronic pelvic pain (male and female)
-
Neuropathic pain (e.g., postherpetic neuralgia)
Advantages Over Pharmacological or Invasive Interventions
Compared to corticosteroids or opioids, SoftWave offers a distinct safety profile:
-
Non-Destructive: There is no risk of tissue atrophy or tendon rupture associated with corticosteroid injections.
-
No Systemic Side Effects: The biological response is local to the treatment area.
-
Repeatable: Treatments can be performed serially to maximize tissue remodeling without the risks of tolerance or addiction.
For the modern clinic, SoftWave offers a tool that addresses the root biology of pain. By acting simultaneously on peripheral nerves, immune signaling, and tissue regeneration, it provides a comprehensive approach to managing complex pain syndromes that resist standard care.
